The road to weight loss is often fraught with difficulties, and trying various diets and supplements with little success can be frustrating. Now, the prescription drug Semaglutide Injections is gaining attention for its significant efficacy in weight management. However, among the many weight-loss adjunctive medications, what makes Semaglutide stand out? This article will delve into its mechanism of action, benefits, and how it can be a turning point on your path to a healthy weight.
What are Semaglutide?
Semaglutide is a prescription medication originally developed for the treatment of type 2 diabetes and has since gained widespread attention for its effectiveness in weight management. It belongs to a class of drugs known as GLP-1 receptor agonists, which work by mimicking a natural hormone released by the body after eating. This hormone plays a key role in regulating appetite, digestion, and blood sugar levels.
Under normal conditions, GLP-1 sends signals to the brain that promote a feeling of fullness and helps slow the emptying of the stomach. In individuals with obesity or metabolic imbalance, this signaling system is often less effective, leading to persistent hunger and overeating. Semaglutide enhances this natural process, allowing people to feel satisfied with smaller portions and reducing the constant urge to eat, without relying on extreme calorie restriction.
Unlike older weight-loss medications that stimulate the nervous system or suppress appetite aggressively, semaglutide works by restoring the body’s own appetite regulation mechanisms. Many users report that they do not feel as though they are “forcing” themselves to eat less; instead, food becomes less dominant in their daily thoughts, making healthier eating patterns easier to maintain over time.
Clinical studies have shown that, when used under medical supervision and combined with lifestyle changes, semaglutide can lead to significant and sustained weight loss for many individuals. Beyond its effects on body weight, it also improves blood sugar control and may reduce certain cardiovascular risk factors, making it particularly beneficial for people with insulin resistance or type 2 diabetes.
That said, semaglutide is not a quick fix or a miracle solution. Some individuals may experience gastrointestinal side effects, especially during the early stages of treatment, and weight regain can occur if the medication is discontinued without lasting changes to diet and lifestyle. For this reason, it is best viewed as a medical tool that supports long-term weight management rather than a short-term dieting aid.
Weekly semaglutide injections
Weekly semaglutide injections are the most common and well-established way this medication is used in clinical practice.
Semaglutide is a long-acting GLP-1 receptor agonist that has been structurally modified to remain active in the body for an extended period of time. Because of its long half-life—approximately one week—it does not require daily dosing. A single subcutaneous injection once per week is sufficient to maintain stable drug levels and provide continuous appetite regulation and metabolic benefits.
One of the key advantages of weekly injections is improved treatment adherence. Compared with daily medications, a once-weekly schedule is easier to maintain over the long term, making it particularly suitable for chronic weight management. The injection is typically administered under the skin of the abdomen, thigh, or upper arm and is designed to be simple enough for most patients to self-administer after proper instruction.
At the start of treatment, the dose is usually increased gradually. This step-up approach allows the body to adjust to the medication and helps reduce gastrointestinal side effects such as nausea or bloating. As the dosage stabilizes, these effects often lessen or resolve.
It is important to understand that although semaglutide is injected only once a week, it is not a one-time or effortless solution. Its effectiveness depends on consistent use over time and works best when combined with healthy eating habits and lifestyle changes. Discontinuing the medication without maintaining these changes may lead to weight regain.
How does semaglutide work?
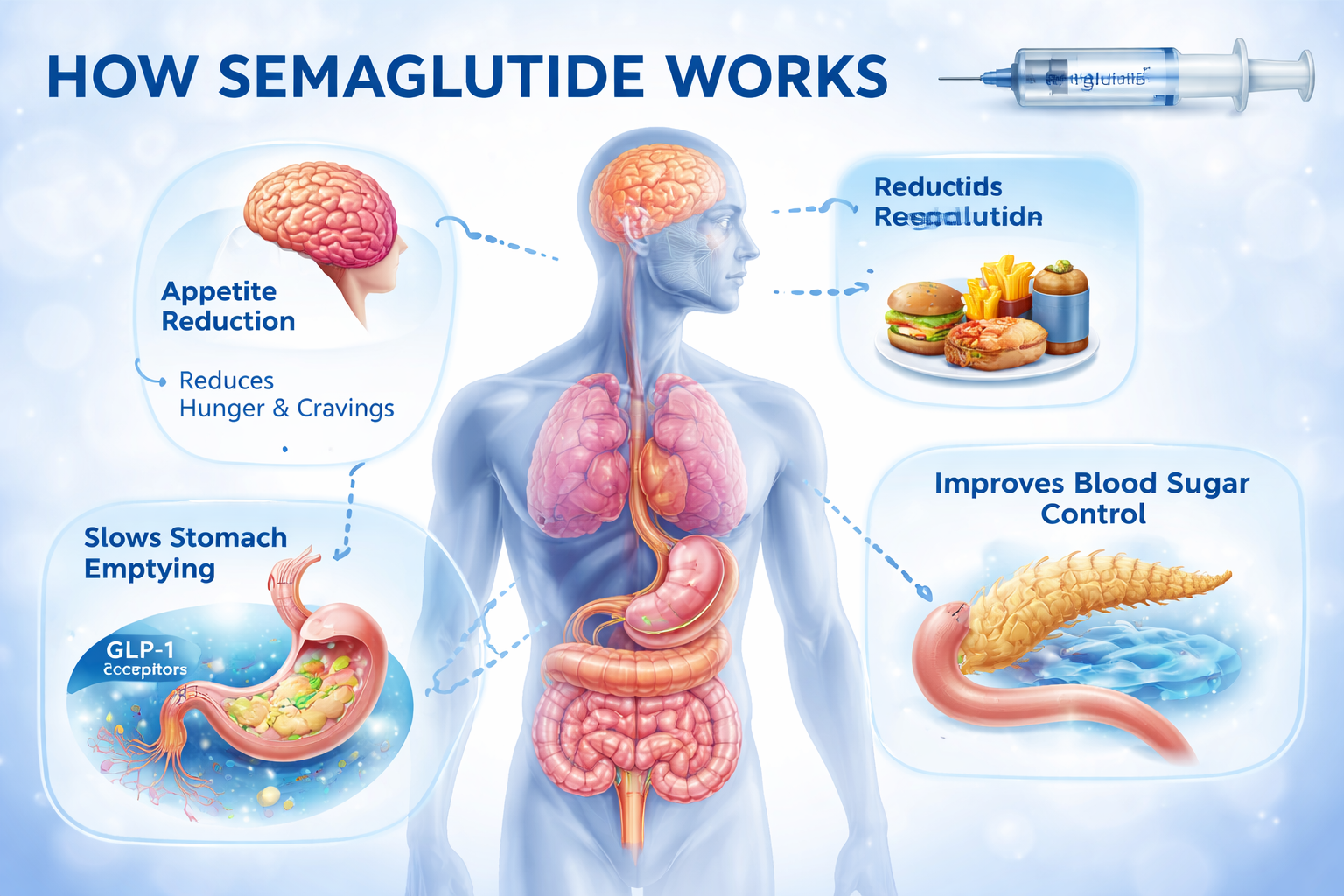
Semaglutide works by enhancing the body’s natural appetite and metabolic regulation systems, rather than forcing weight loss through stimulation or extreme restriction.
Semaglutide is a GLP-1 (glucagon-like peptide-1) receptor agonist, meaning it mimics a hormone that the body naturally releases after eating. GLP-1 plays a central role in signaling fullness to the brain, regulating digestion, and controlling blood sugar levels. By activating GLP-1 receptors, semaglutide prolongs and strengthens these signals.
In the brain, semaglutide acts on appetite-regulating centers to reduce hunger and decrease food cravings. As a result, many people experience a noticeable drop in appetite and feel satisfied with smaller portions. Food becomes less mentally dominant, which helps reduce overeating and emotional eating.
In the digestive system, semaglutide slows gastric emptying, allowing food to remain in the stomach longer. This extends the feeling of fullness after meals and reduces the urge to eat frequently, while also helping to stabilize post-meal blood sugar levels.
From a metabolic perspective, semaglutide improves insulin response when blood glucose rises and suppresses excessive glucagon release. This leads to better blood sugar control and fewer energy fluctuations that can drive hunger and fat storage.
Overall, semaglutide does not directly burn fat. Instead, it reduces appetite, prolongs satiety, and improves metabolic balance, making it easier to consume fewer calories in a sustainable way. This biology-based mechanism is what sets semaglutide apart from traditional weight-loss approaches and supports more durable results over time.
What are the research results regarding semaglutide?
Research on semaglutide has shown that it has significant effects on both weight management and metabolic health. Large clinical trials, such as the STEP series, demonstrated that weekly administration of 2.4 mg semaglutide combined with a reduced-calorie diet led to an average weight loss of about 15% over 68 weeks, with some participants losing even more than 20% of their body weight. Beyond weight reduction, semaglutide improves blood sugar control, lowering fasting glucose and HbA1c levels, and also has beneficial effects on blood pressure and lipid profiles. Studies further indicate that it markedly reduces hunger, diminishes cravings for high-calorie foods, and decreases episodes of overeating, consistent with its mechanism of action in regulating appetite centers in the brain and slowing gastric emptying. Overall, semaglutide not only supports substantial weight loss but also improves overall metabolic health, making it a scientifically grounded and sustainable option for long-term weight management. Common side effects are mainly gastrointestinal, such as nausea or vomiting, usually occurring during the initial phase of treatment and often easing as the body adapts.
Semaglutide side effects
Semaglutide is generally well tolerated, but like all medications, it can cause side effects. Most of these are related to the gastrointestinal system, with a few rare but more serious reactions reported.
Common Side Effects
1. Nausea: The most frequently reported side effect, usually occurring during the early stages of treatment
2. Vomiting, bloating, diarrhea, or constipation: Typically mild to moderate and often decrease as the body adjusts
3. Reduced appetite: While this is part of the drug’s intended effect, it can sometimes be accompanied by mild discomfort
Rare or Serious Side Effects
1. Pancreatitis: Rare, but has been reported in association with GLP-1 receptor agonists
2. Gallbladder issues: Such as gallstones, especially with long-term use
3. Hypoglycemia: Risk is low when used alone but can increase if combined with insulin or sulfonylureas
4. Thyroid C-cell tumors: Observed in animal studies; semaglutide is not recommended for individuals with a personal or family history of medullary thyroid carcinoma (MTC)
Safety Considerations
1. Gradual dose escalation: Starting with a low dose and increasing slowly can significantly reduce nausea and gastrointestinal discomfort
2. Medical supervision: Pre-treatment evaluation should consider personal history of pancreatic, gallbladder, or thyroid disorders
3. Monitoring: Patients should monitor blood glucose and report any unusual symptoms during treatment
Overall, most side effects of semaglutide are manageable, short-term, and tend to decrease as the body adapts. Proper dose adjustment and medical guidance are key to minimizing risks.
What should be noted when using Semaglutide?
When using semaglutide, it is important to consider safety and individual health factors to ensure both effectiveness and tolerability. Before starting treatment, personal and family medical history should be assessed, particularly regarding thyroid disorders (such as medullary thyroid carcinoma or multiple endocrine neoplasia type 2), pancreatic disease, and gallbladder health. The medication is typically initiated at a low dose and gradually increased to the therapeutic dose to minimize side effects such as nausea, vomiting, or gastrointestinal discomfort. Blood glucose should be monitored, especially when used alongside insulin or sulfonylureas, and patients should watch for signs of pancreatitis or gallbladder issues. Semaglutide is not recommended for pregnant or breastfeeding women, nor for children. For optimal results, it should be combined with a healthy diet and regular physical activity under medical supervision. Discontinuation without maintaining lifestyle changes may lead to weight regain, so long-term management still relies on sustained healthy habits.
Semaglutide is a clinically approved medication designed to help obese adults manage their weight. It belongs to the GLP-1 receptor agonist class and targets and activates glucagon-like peptide-1 receptors in the gut. This mechanism primarily produces two effects: significantly reducing appetite and regulating blood sugar levels. For patients with type 2 diabetes, semaglutide also offers the advantage of aiding in glycemic control. However, it is important to note that despite its numerous benefits, the effects of this medication are not immediate. Patients may experience the effects several hours after taking the medication. If you are looking for a comprehensive weight management program or better glycemic control, semaglutide is undoubtedly a reliable option, manufactured in our factory laboratory in China.
Semaglutide is a GLP-1 receptor agonist that supports weight loss through several mechanisms. It acts on the brain’s appetite centers, helping people feel full faster and thereby reducing food intake. It also slows gastric emptying, which prolongs post-meal satiety, decreases snacking, and helps stabilize blood sugar levels. Additionally, semaglutide promotes insulin secretion, suppresses glucagon release, and improves insulin sensitivity, benefiting both blood sugar control and weight management. Clinical studies show that overweight or obese individuals, when combined with a healthy diet and regular exercise, can lose an average of 10–15% of their body weight over six months to a year. By reducing appetite, extending feelings of fullness, and enhancing metabolism, semaglutide provides a safe, effective, and sustainable approach to weight loss.
Tirzepatide and Semaglutide are both injectable medications for type 2 diabetes and obesity, but they work differently: Semaglutide is a GLP-1 receptor agonist, while Tirzepatide is a dual GIP/GLP-1 receptor agonist. Overall, Tirzepatide generally provides greater blood sugar reduction and weight loss but may cause slightly more gastrointestinal side effects. Semaglutide has a longer track record with more established long-term safety data. Choice depends on individual goals: Tirzepatide may be preferred for maximum weight loss and strong glucose control, while Semaglutide may be better for tolerability and long-term safety.
The key distinction lies in their mechanisms of action. Although both are incretin mimetics, semaglutide is a GLP-1 receptor agonist, whereas tirzepatide acts on both GLP-1 and GIP receptors. This dual action may render tirzepatide more effective in promoting weight loss and improving glycemic control.
Semaglutide should be administered once a week, on the same day each week. Consistency is important to maintain stable drug levels in your body and optimize its effectiveness for weight management or blood sugar control.
Early research suggests that retatrutide works faster because it activates multiple pathways that affect appetite, energy expenditure, and fat burning. Many trial participants experienced changes in appetite and weight much earlier than those using semaglutide.
About Gentolex
Gentolex’s goal is to create opportunities connecting the world with better services and guaranteed products. Up to date, Gentolex Group has been serving customers from more than 10 countries, specially, representatives are established in Mexico and South Africa. Our main services focus on supplying peptides APIs and Custom Peptides, FDF license out, Technical Support & Consultation, Product Line and Lab Setup, Sourcing & Supply Chain Solutions.
With the passion and ambition of our teams, comprehensive services have been fully set up. To continue serving customers worldwide, Gentolex is already engaged in manufacturing, sales & distribution of pharma ingredients. At present, we are allocated with:
For pharma ingredients, we have shared holding a lab and CMO facility for Peptide APIs development and manufacturing, and in order to offer an extensive range of APIs and intermediates for development study and commercial submission to satisty varieties of customers, Gentolex also adoptes a model with signing strategic cooperation with strong manufacturing sites who have national platforms for drug research, technology innovation and production, passed GMP inspection of NMPA (CFDA), US FDA, EU AEMPS, Brazil ANVISA and South Korea MFDS, etc, and owns tech and know-how for the widest range of APIs. Documents (DMF, ASMF) and certificates for registration purpose are ready to support. The main products have been applied to Digestive diseases, Cardio-vascular system, anti-diabetes, Antibacterial and antiviral, Antitumor, Obstetrics and Genecology, and Antipsychotic, etc. All high-quality products are rigorously tested before being delivered in drums, bags or in bottles. We also provide additional value to customers through our refilling or repacking services.
All our manufacturers have been inspected by our team to ensure they are qualified for international markets. We accompany customers or on behalf of our customers to conduct additonal due diligence on manufacturers upon requests.
For chemical products, we are joint-venture of 2 factories in Hubei and Henan provinces, an overall construction area of 250,000 square meters under international standard, products covering Chemical APIs, Chemical intermediates, Organic chemicals, Inorganic chemicals, Catalysts, Auxiliaries, and other fine chemicals. The management of factories enables us to offer flexible, scalable and cost-effective solutions across a wide variety of products to serve global clients.
Post time: Dec-23-2025


